Navigating the turbulent waters of a child’s emotional life is arguably one of the most challenging aspects of parenting. When a child has a meltdown — the screaming, the tears, the complete loss of control — it’s natural for a parent or carer to feel their own stress levels spike. But understanding what a meltdown truly is, moving beyond seeing it as mere misbehavior, and knowing how to effectively help your child recover is the bedrock of teaching them emotional resilience.
A meltdown is a sign that a young person is completely overwhelmed—their internal resources for managing feelings like anger and frustration have been exhausted, often due to sensory overload or emotional exhaustion. Learning to stay calm yourself and providing a safe, predictable response is crucial. Our guide is here to equip parents and carers with the expert tools and compassionate understanding needed to defuse these powerful emotional outbursts and build a stronger, more trusting connection with their child.
What Happens During a Meltdown
Understanding the distinction between a typical temper tantrum and a genuine meltdown is the first step toward effective support. While both involve distressing outbursts, the underlying cause and the young person’s level of control are fundamentally different. It’s essential for parents and carers to recognise the signs early so they can offer the right kind of help and support.
Common Signs of a Meltdown
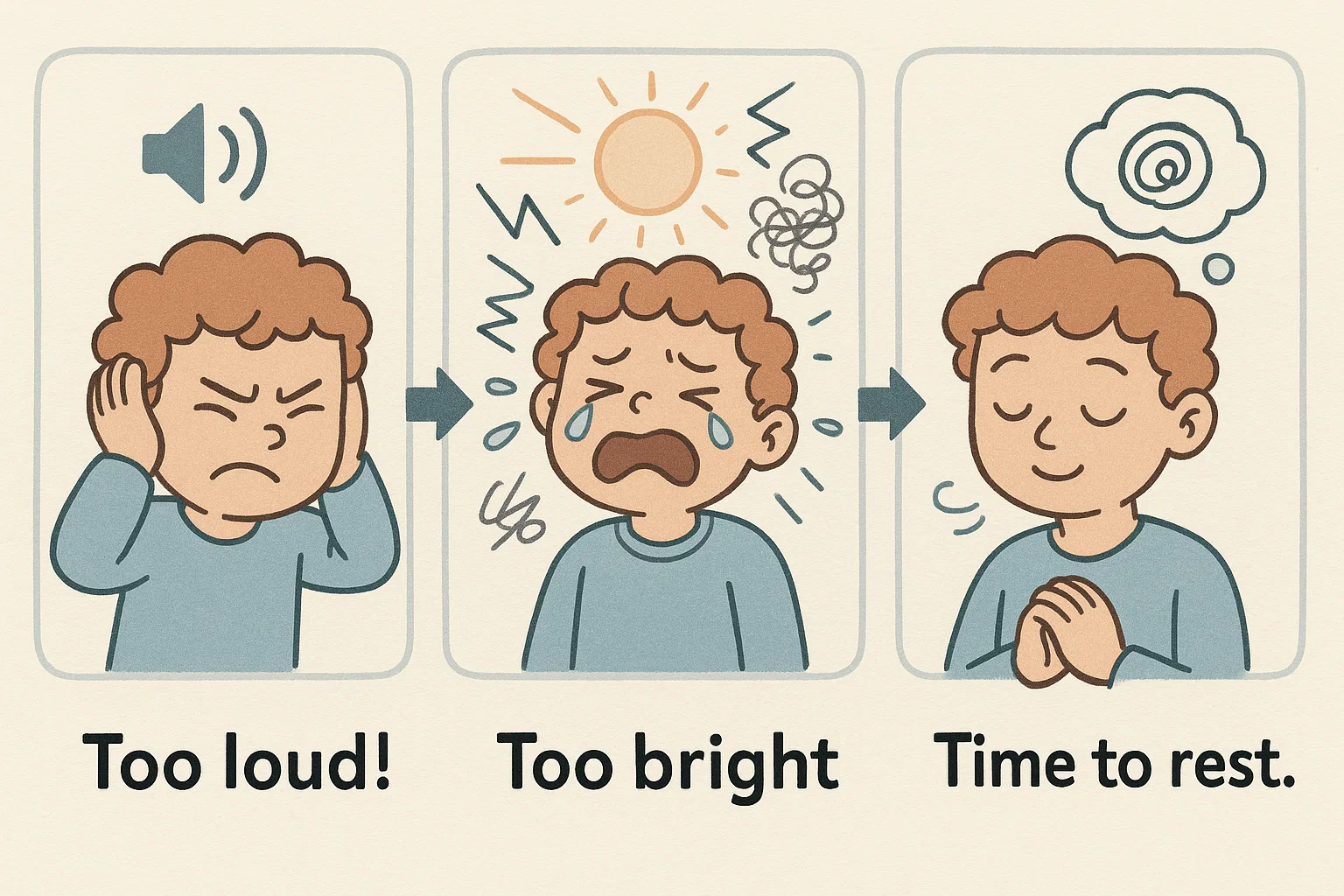
Meltdowns are characterized by a total loss of emotional and behavioral control, stemming from an overwhelmed nervous system. These emotional outbursts aren’t deliberate; they are a response to being overstimulated.
Physical and emotional indicators that a young person may be spiraling toward a meltdown include:
- Intense, inconsolable crying or screaming: The sound is often distressed and panicked, not manipulative.
- Covering ears or eyes: This is a clear indicator of sensory distress, particularly from loud noises or bright lights.
- Physical escalation: Pacing, hitting, kicking, or throwing objects.
- Shutting down or withdrawing: The distressed person may withdraw into themselves, become non-verbal, or freeze.
- Repetitive behavior (Stimming): Actions like rocking or fidgeting to try and self-regulate.
- Refusal to be touched or spoken to: They are often overwhelmed by external stimuli.
Meltdown vs Tantrum
The terms meltdown and tantrum are often used interchangeably, but they represent two different types of emotional expression, particularly among toddlers and young children.
| Feature | Meltdown | Tantrum (Temper Tantrums) |
| Origin | Overwhelmed nervous system; loss of control. | Goal-oriented; a way to communicate a want/need. |
| Control | No control; the individual is truly suffering. | Some control; behavior stops when goal is achieved (e.g., gets the toy). |
| Triggers | Sensory overload, emotional exhaustion, anxiety. | Frustration over boundaries, denied requests. |
| Response | Needs co-regulation, safety, and a quiet space. | Needs firm, calm boundaries and often ignoring the performance. |
| State | Completely overwhelmed and disorganized. | Frustrated but aware of their surroundings. |
Why Meltdowns Happen
When meltdowns happen, they are often a clear signal that the young person’s resources for managing their world have run out. Understanding the trigger is vital to effectively support your child.
Key reasons why a youth’s meltdown may occur include:
- Sensory Overload: The brain is unable to process the amount of information coming from their senses. A busy supermarket, bright lights, or loud noises can all lead to an overwhelmed system.
- Frustration: A young person is getting frustrated because they lack the language or motor skills to complete a task or communicate a critical need. This is especially true when they aren’t able to articulate what they want.
- Anxiety and Fatigue: Lack of sleep, hunger (give your child a healthy snack), or an underlying worry can significantly lower the emotional threshold.
- Routine Change: Unexpected transitions or deviations from a predictable schedule can make kids feel insecure and lead to feeling overwhelmed.
Steps to Calm Kids After a Meltdown
Once the intense phase of the outburst has passed, the goal shifts from simply surviving the moment to fostering safety, connection, and recovery. The post-meltdown phase is critical for helping the child learn self-regulation.
Ensure Safety First
Your absolute top priority is to keep the young person and everyone around them safe.
- Move to a quieter and safer area if possible. If you are in a crowded place, gently guide the individual away from people and sharp objects.
- Remove any immediate physical threats. This includes making sure they cannot fall down stairs or run into traffic.
- Do not try to reason or withhold comfort. Physical restraint should be avoided unless absolutely necessary to prevent injury. The focus is not on punishment but on safety and containment.
Stay Calm and Grounded
As the parent or carer, your response is the anchor. If you become frantic, their distress will escalate.
- Deep Breaths: Take a few deep breaths yourself. This helps you regulate your own nervous system so you can stay calm. A dysregulated adult cannot help a dysregulated child regain control.
- Speak Softly: Use a low, monotone voice. Too much stimulation from your voice can be jarring.
- Use Neutral Body Language: Avoid aggressive or frustrated postures. Kneel down to their level, maintaining a safe, open stance. Being a calmer presence helps the person feel secure.
Give Space and Time
Once safety is ensured, remember that immediate interaction might feel like a further invasion to someone who is feeling overwhelmed.
- Allow Decompression: Sometimes, the best thing you can do is sit quietly nearby. Let your child process the intense emotional energy without pressure.
- Do Not Force Communication: Do not demand an explanation or apology right away. Their cognitive brain is not online yet. Wait until your child moves from intense crying to quiet attention or calm breathing.
Offer Comfort and Reassurance
When the intensity subsides, connect through gentle, non-demanding methods.
- Gentle Touch: If receptive, a gentle hand on the back or an embrace can be incredibly grounding. Note: Some individuals, especially those with sensory processing challenges, may reject touch during or immediately after an outburst.
- Safe Space: Offer a comforting object like a special blanket, a favorite stuffed animal, or suggest a safe space like a calm corner or a quiet room.
- Sensory Input: A drink of cool water, a quiet period of listening to music with noise-canceling headphones, or a weighted lap pad can provide necessary input to help stabilize their system.
Talk Later — Not During
The primary rule in dealing with child meltdowns is: Don’t try to reason with them while they are actively losing control.
- Wait for Recovery: Discuss the event only after the individual has fully recovered, perhaps 20 minutes to an hour later. The frontal lobe (the part of the brain for logic) needs time to come back online.
- Short, Simple Sentences: When you do talk, keep it brief and focused on validation before problem-solving. Tell your child you saw how upset they were.
| Recovery Stage | Parent/Carer Focus | Actionable Strategy |
| Active Meltdown | Safety and regulation. | Quietly maintain safe proximity, deep breaths. |
| Post-Meltdown (Minutes) | Comfort and reconnection. | Gentle touch (if receptive), offer water, move to a quieter spot. |
| Recovery (15+ Minutes) | Validation and reflection. | Talk with your child about the feeling, not the behavior. |
Helping Kids Recover Emotionally
The period after the meltdown is your opportunity to teach emotional intelligence, often referred to as “co-regulation.” This is where the child learns the essential skills to be better able to manage their emotions next time.
Validate Feelings
Validation is not condoning the behavior; it is acknowledging the genuine pain and overwhelm the individual experienced.
- Name the Feeling: Remind your child what the big emotion was. You can say, “You were feeling completely overwhelmed when the music was too loud,” or “That was a big wave of anger and frustration.”
- Acknowledge the Difficulty: Help them feel understood by saying things like, “It’s really hard when things don’t go the way you planned.” This helps the child talk about the experience without fear.
Encourage Expression
After the individual is calmer, offer healthy, age-appropriate ways to process the leftover feelings.
- Creative Outlets: Encourage drawing a picture of the “monster feeling,” journaling, or using play figures to act out what happened.
- Use Pictures: For toddlers and young children, use pictures or an emotion chart to point to how they felt, as they might not have the language yet.
- Talk About it: When they are ready, let your child know you are ready to listen without judgment. Listening to music can also be a gentle way to shift the mood.
Avoid Blame or Shame
Never make a person feel bad about the meltdown itself. Meltdowns are a form of distress, not malice.
- Focus on the Future: Instead of dwelling on the negative behavior, focus on the strategy. “Next time you feel your body getting hot and tight, what tool from your toolkit can we use?”
- Highlight Resilience: Tell your child you are proud of them for calming down, even though it was hard. The individual might feel embarrassed or ashamed, so your positive focus is vital. Let your child know that everyone struggles to manage difficult emotions sometimes. The key is what they do afterward.
Preventing Future Meltdowns
The long-term goal for parents and carers is to reduce the frequency and intensity of these episodes. This involves identifying your child’s triggers and proactively teaching calming strategies.
Identify Triggers
Help parents notice patterns by keeping a simple log of when and where the meltdowns occur.
- Meltdown Diary: Note the time of day, location (crowded, noisy), activity before the meltdown, how much sleep was had, and what was eaten. This helps you figure out what to recognise in the future.
- Look for Themes: You may find that meltdowns cluster around transitions, hunger, or specific social situations. This insight allows you to prevent the environment from overwhelming them.
Build Predictable Routines
Consistency is a key element in helping children feel secure and in control.
- Schedule Reliability: Maintain consistent times for sleeping, waking, and meals.
- Prepare for Transitions: Give your child advanced notice (5-10 minutes) before a transition, like leaving the playground. You can say, “In five minutes, we will be leaving.”
Teach Coping Tools
These are the strategies that help the child calm down before the point of no return. The young person needs to practice these tools when they are calm so they have them when they are not.
- Deep Breathing Techniques: Teach fun names like “balloon breathing” (blowing up a balloon) or “star breathing” (tracing a star shape while inhaling and exhaling).
- “Calm-Down Corner”: Set up a designated area with pillows, books, sensory toys, or a weighted lap pad where the individual can choose to go when they feel their emotions rising.
- Sensory Items: A fidget toy, a chewy necklace, or a stress ball can provide a healthy outlet for rising frustration.
Use Visual Supports
Visuals are a powerful way to reduce anxiety, particularly for those who struggle to manage change or uncertainty.
- Visual Schedules: Pictures showing the day’s activities can help a young person know what to expect.
- Emotion Charts: A chart showing different facial expressions allows the person to point to how they feel, even if they can’t articulate it. This is helpful when the child knows they are feeling something but cannot put it into words.
Supporting Children with Sensory or Emotional Sensitivity

For children with developmental differences like Autism Spectrum Disorder (ASD), ADHD, or Sensory Processing Disorder (SPD), meltdowns often involve genuine sensory overload and require specialized approaches.
Create a Sensory-Friendly Environment
Small changes to the environment can have a massive impact on a child’s behaviour and the individual’s triggers.
- Light and Sound: Use dimmer switches and natural light where possible. Minimize exposure to loud noises in the home and provide noise-canceling headphones for outings.
- Clothing and Textures: Pay attention to clothing tags, seams, or irritating fabrics. Let your child choose comfortable clothes that don’t cause distress.
Offer Sensory Breaks
These breaks are not a reward or a punishment; they are a necessary reset for an overwhelmed nervous system.
- Movement Breaks: Allow movement that provides deep pressure or vestibular input, such as jumping, climbing, or swinging.
- Quiet Decompression: Schedule short, mandatory quiet times during the day, even if the person doesn’t seem stressed. Think of it as preventative maintenance.
Collaborate with Therapists
Health professionals like Occupational Therapists (OTs) and Behavioral Specialists can provide individualized strategies.
- OT Support: An OT can conduct a sensory profile assessment and design a “sensory diet”—a personalized plan of activities and input to help the system stay regulated throughout the day.
- Behavioral Support: A specialist can help develop a comprehensive plan to manage meltdowns and tantrums, focusing on communication skills and coping mechanisms.
When to Seek Professional Help
While all young people experience intense emotions, frequent, severe, or lengthy meltdowns that disrupt family life or impact the individual’s functioning may signal a need for support from professionals.
Talk to a Pediatrician or Child Psychologist
If you are consistently struggling to manage your child’s emotional regulation, it’s time to consult an expert.
- Assessment: Professionals can assess for underlying issues such as high anxiety, ASD, ADHD, or SPD.
- Interventions: They can recommend tailored interventions, including cognitive-behavioral therapy (CBT) for anxiety, or specific behavioral protocols.
Explore Family or Parent Coaching
Sometimes, the parents need the toolkit as much as the individual does.
- Parent Training: Programs focused on emotional regulation and responsive parenting techniques can provide practical, concrete strategies for dealing with child meltdowns and building a calmer household environment.
Watch for Signs of Deeper Distress
Be aware of accompanying symptoms that suggest more than typical toddlers and young children boundary-testing.
- Red Flags: Watch for persistent changes in sleep or appetite, frequent complaints of headaches or stomach aches, a person who wants to avoid school or social events, or expressing significant worry that is disproportionate to the situation.
Taking Care of Yourself as a Parent

It’s physically and emotionally exhausting to be a parent or carer who is constantly dealing with child meltdowns. Your ability to stay calm is directly linked to your own well-being.
Manage Your Own Stress
You cannot pour from an empty cup. Prioritizing your own regulation is the most effective way to support your child.
- Self-Care: Schedule small, non-negotiable moments of rest, whether it’s a few minutes of quiet sitting, a hobby, or even just stepping away for a 5-minute breather.
- Realistic Expectations: Accept that perfection is impossible. There will be tough days. Remind your child and yourself that you are both learning.
Build a Support Network
- Connect with Others: Talk to trusted friends, family, or professional therapists. Joining support groups with other parents and carers facing similar challenges can ease feelings of isolation.
Remember Progress Takes Time
Emotional regulation is a skill, not an inherent trait. It takes years to develop fully.
- Celebrate Small Wins: Notice and celebrate when the child’s behaviour is even slightly better managed, or when you were able to stay calm for longer. Every small step forward builds confidence and resilience for both you and your child.


